Behavioral Healthcare Design: Key Design Variables
In our last blog we discussed the current and future changes seen in the behavioral healthcare design industry. We’re now ready to move on to discussing key design variables that are currently being studied. Our final post in this three-part series will discuss the five key factors to consider for patient well-being when designing these facilities.
Understanding the Complexity of Behavioral Healthcare Design
Therefore, like Corrections, leading planners and designers specializing in Behavioral Healthcare are delving deeper to better understand the complexity of issues and to be the activist to design facilities that promote treatment and healing – and a safer community.
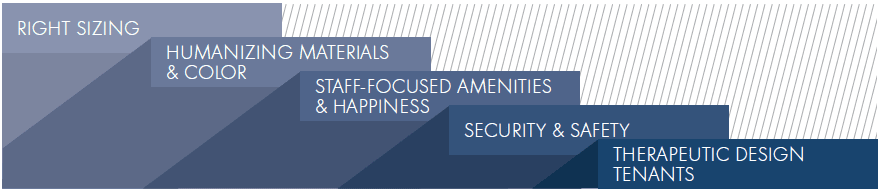
The following is a list of key design variables that are being studied and implemented:
- Right Sizing
- Humanizing Materials and Color
- Staff-Focused Amneties and Happiness
- Security and Safety
- Therapeutic Design Tenants
Right-sizing
Today’s Behavioral Healthcare facilities are often one-story single buildings within a campus size. Often debated by Clients due to costs, this design preference is driven by the demand for natural light, window views to nature for all patient areas, and outdoor open-air gardens “wrapped” within. All of this provides soothing qualities to the patient, reduces their anxieties, counteracts disruptive conduct and helps to reduce staff stress.
“When you look at the program mix in these buildings, there’s a high demand for perimeter because there are a lot of rooms that need natural light. Offices, classrooms, dining areas, community rooms, and patient rooms all demand natural light, so you end up with a tremendous amount of exterior wall, and it forces the building to have a very large footprint.” – James Kent Muirhead, AIA, associate principal at Cannon Design in Baltimore
These design principles are also believed to improve staff work conditions. Unlike a multi-story complex, at any moment staff can walk outdoors and access nature, free from visual barriers, and within a building that more accurately reflects building types that both patients and staff would encounter in their communities.
In addition to right-sizing for the overall building footprint, is right-sizing for internal patient and staff support area. Similar to the move we have seen in Corrections to de-centralize support spaces, Behavioral Healthcare is moving to decentralized nursing/patient units called “neighborhoods.” With mental health facilities there is a large concern with distances and space adjacencies in relation to the patient room and patient support areas such as treatment and social spaces. Frank Pitts, AIA, FACHA, OAA president of Architecture Plus, Troy, NY, advocates neighborhoods that average 24-30 beds arranged in sub-clusters, called “houses”, of 8-10 beds. Thus, each neighborhood consists of three houses. Often these layouts will include a common area where patients congregate and socialize, with a separate quiet room so patients can elect to avoid active, crowded areas. In addition Pitts states, “There’s a move away from central dining facilities. So, while facilities will still have a central kitchen, it’s a whole lot easier moving food than it is patients.” However, it is important for the facility to mimic normal outside daily life routines, so patients are encouraged to frequently leave their neighborhoods to attend treatment sessions, and outdoor courtyards.
Humanizing Materials & Color
In all facilities that play a role in rehabilitation, design strives to create spaces that humanize, calm, and relax. Behavioral Healthcare patients need to feel that they are in familiar surroundings; therefore, the architectural vocabulary should feel comfortable and normal. Since these facilities are about rehabilitation (when possible) and encouraging patients to merge back into society, the facility should feel like an extension of the community. Their spaces should reflect the nature and architecture of the surrounding region and thus so, no two facilities should look too much alike.
“Our approach to designing these facilities is to view the facility as an extension of the community where patients will end up when they’re released. Interior finishes also depend on geography because you want to replicate the environment patients are used to. You want to de-stigmatize the facility as much as possible.” – Tim Rommel, AIA, ACHA, OAA, principal with Cannon Design in Buffalo, NY.
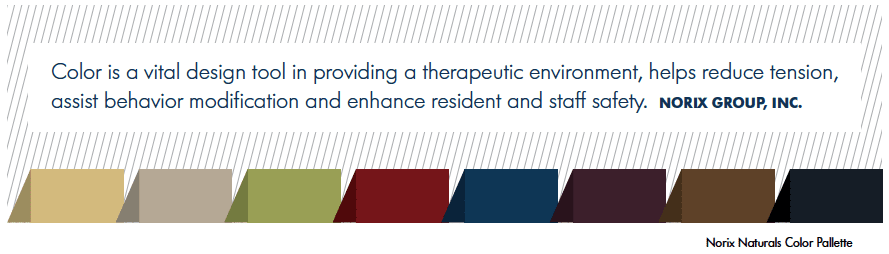
Therefore, materials and colors within these spaces want to feel familiar to one’s region and everyday life. To soothe the psyche and rehabilitate, they want to feel soft and comfortable, yet visually stimulating. An interior that is overly neutral or hard in appearance is not appropriate. Materials should reduce noise, and colors should lift the spirit. This can help to create an environment in which the patient can learn, socialize, and be productive while easing anxieties, delivering dignity, and modifying behavior. As stated previously, behavioral studies advise the use of softer interior materials—like carpeting, wood doors and tile. Doing so translates directly to both patient and staff well-being, particularly staff safety, and makes for a nicer place to work. In addition, staff have more resources to “treat” instead of manage heated situations. When staff experiences are eased and satisfied, morale is boosted and life-saving rules and policies are more likely to be enforced.
Staff-Focused Amenities & Happiness
While reducing staff stress and fatigue through a healing supportive environment seems like an obvious goal, there are relatively few studies that have dealt with this issue in any detail. More attention has been given to patient outcomes. However, many leading hospitals that have adopted therapeutic tenants into their newly built environments have seen vast improvement through their “business matrixes” and financial reporting.
In one example, the Mayo Clinic, a national leader in implementing healing design in its facilities, has reported a reduction of nursing turnover from a national annual average of 20% to an annual 3%-4%. In another example, when Bronson Methodist Hospital incorporated evidence-based design into its new 343-bed hospital, they cited their 19%-20% nurse turnover rate dramatically dropped to 5%.
Now, both the Mayo Clinic and Bronson Methodist Hospital have had to initiate a waiting list for nursing staff seeking positions. This converts to better-trained and qualified staff, and a reduced error rate. Therefore, more health facilities are investing in staff support areas such as lounges, changing rooms, and temporary sleep rooms. Within these staff spaces and in the hospital throughout, facilities are also recognizing the need for upgrade materials, better day lighting, and an interesting use of color: One soon realizes that the need of patients and staff are interwoven, each impacting positively or negatively the other.
Security & Safety
Without debate, self harm and harm to staff is one of the biggest concerns mental health facilities manage. Often the biggest safety and security concern is the damage patients can do to themselves. “There are three rules I had drummed in me,” says Mark Hanchar; Director of Preconstruction Services for Gilbane Building Company, Providence, R.I. “First, there can’t be any way for people to hang themselves. Second, there can be no way for them to create weapons. Third, you must eliminate things that can be thrown.” Hanchar says that the typical facility is, “a hospital with medium-security prison construction.” This means shatter proof glass, solid surface countertops (laminate can be peeled apart), stainless steel toilets and sinks (porcelain can shatter), push pull door latches and furniture that cannot be pulled apart and used as a weapon. These are just to name a few.
Additionally, removing barriers between patients and nursing staff is a safety consideration. Frank Pitts, AIA, FACHA, OAA president of Architecture Plus, says what may be counter-intuitive for safety precautions, “Glass walls around nursing stations just aggravate the patients.” Removing glass or lowering it at nursing stations so patients can feel a more human connection to nurses often calms patients. There is also discussion of removing nursing stations altogether; decentralizing and placing these care needs directly into the clinical neighborhoods and community spaces. Pitt says, “The view is that [nursing staff] need to be out there treating their patients.”
Therapeutic Design Tenants
 As medicine is increasingly moving towards “evidence-based” medicine, where clinical choices are informed by research, healthcare design is increasingly guided by research linking the physical environment directly to patient and staff outcomes. Research teams from Texas A&M and Georgia Tech sifted through thousands of scientific articles and identified more than 600 – most from top peer-reviewed journals – to quantify how hospital design can play a direct role in clinical outcomes.
As medicine is increasingly moving towards “evidence-based” medicine, where clinical choices are informed by research, healthcare design is increasingly guided by research linking the physical environment directly to patient and staff outcomes. Research teams from Texas A&M and Georgia Tech sifted through thousands of scientific articles and identified more than 600 – most from top peer-reviewed journals – to quantify how hospital design can play a direct role in clinical outcomes.
The research teams uncovered a large body of evidence that demonstrates design features such as increased day-lighting, access to nature, reduced noise and increased patient control helped reduce stress, improve sleep, and increase staff effectiveness – all of which promote healing rates and save facilities cost. Therefore, improving physical settings can be a critical tool in making hospitals more safe, more healing, and better places to work.
Today’s therapeutic spaces have been defined to excel in 3 categories:
- Provide clinical excellence in the treatment of the body
- Meet the psycho-social needs of patients, families, and staff
- Produce measurable positive patient outcomes and staff effectiveness
Considering the cost of treating mental illness, which is exceedingly high, and wanting facilities to have effective outcomes, a further practice of incorporating therapeutic design is increasing. The National Institute of Mental Health (NIM H) approximated in 2008 that serious mental illnesses (SMI ), costs the nation $193 billion annually in lost wages. The indirect costs are impossible to estimate.
The estimated direct cost to clinically treat is approximately $70 billion annually and another $12 billion spent towards substance abuse disorders. In addition to the increased need of care and the boom in Behavioral Healthcare construction, it becomes an obligation to make certain that we as facility managers, architects, designers and manufacturers therapeutically plan and design these facilities.
Additional Information
The information contained in this excerpted post is intended as a guide for architects, specifiers, designers, facility planners, medical directors, procurers, psychologists and social workers which have a stake in providing improved facilities for behavioral healthcare patients. It is a portion of a full report entitled “The Contributions of Color” authored by Tara Hill, of Little Fish Think Tank.
Ms. Hill was commissioned by Norix Group Inc., in 2010 to research the role color plays in the safe operation of correctional facilities and behavioral health centers. More in-depth information specifically about the psychological influence of color and behavioral healthcare facility design can be found by reading the full report.
Do you hahttps://norix.com/resources/white-papers/role-color-humanizing-behavioral-healthcare/ve friends or colleagues who are interested in behavioral healthcare design? If they are interested in current key design variables, be sure to share this post with them using the Facebook, Twitter, Google and share buttons below. Stay tuned for our final post in this three-part series on behavioral healthcare design. Don’t hesitate to share your feedback and experience on this industry in the comment section below.